Grantee Spotlights

Bivona Child Advocacy Center Marks Child Abuse Prevention Month With Major Announcement!
April is Child Abuse Prevention Month and Bivona Child Advocacy Center has announced a second location and expanded services for the community!
The new location in Irondequoit is set to open in the fall of 2024. Services will include community education for school districts and will grow to include new mental health services for survivors and families along with trainings specifically for parents at high risk of abuse and neglect.
The Health Foundation is proud to partner with Bivona and other funders in support of this expansion designed to improve equity and access to services — ensuring children are supported and positioned for long-term success. Browse resources and information about Child Abuse Prevention Month on Bivona’s website.
United Way Celebrates 60th Anniversary in Orleans County
Thank you to the United Way of Orleans County for inviting Program Officers Hannah Castelli and Rachel Betts to attend the recent Friendraising Event at the historic Bent’s Opera House in celebration of 60 years of service!
Since 2021, the Health Foundation has supported the United Way of Orleans following the merger with five other rural United Ways completed to strengthen their ability to respond to additional hardships that the COVID pandemic had created for them and for their community partners. This collaboration seeks the resources and expertise to support community collaborations, collaborative grant seeking and development of community wide fund-raising events within the United Way and local community-based organizations to increase resources within the region.
Read more in this Orleans Hub news article here.

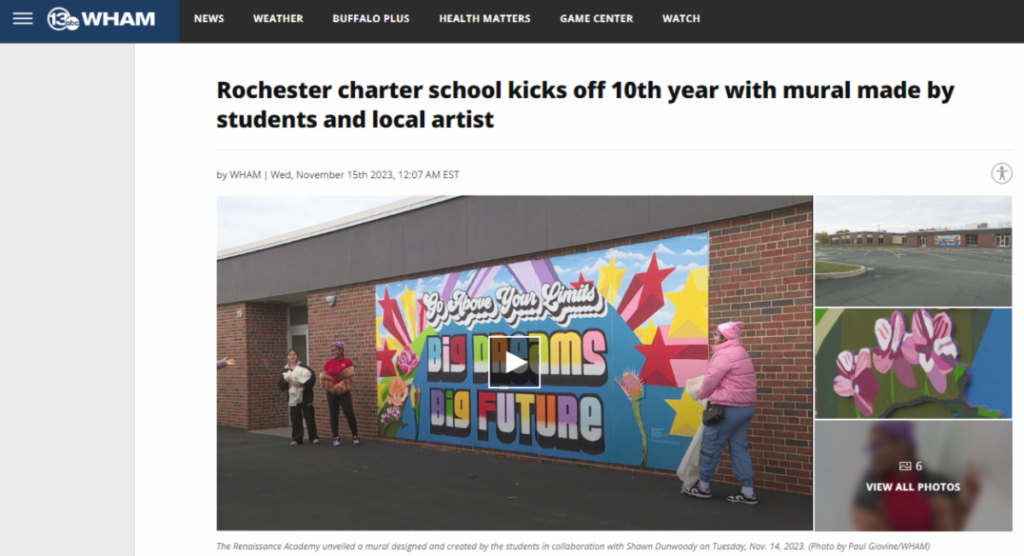
Renaissance Academy Charter School
Congratulations to Renaissance Academy Charter School of the Arts, celebrating its 10th year as a school with the unveiling of the “Decade of Dreams” mural by Shawn Dunwoody, in collaboration with students.
The event included performances by the school choir and a Q&A session with one of the student mural artists. The event was featured on 13 WHAM News.
Renaissance Academy Charter School of the Arts is a 2003 Health Foundation grantee. We are proud to support the school in its efforts to to bolster its efforts to address trauma and systemic barriers via mental health support services for students.
University of Rochester Medical Center
The University of Rochester Medical Center has announced a first-of-its-kind initiative to improve health care access and wellness outcomes in rural communities in Upstate New York through the distribution of telehealth stations conveniently located at local bank branches. Woven into the fabric of rural towns, banks offer the ideal physical location to bridge the geographic divide between patients and providers, offering a vital touchpoint to reach an underserved population.
The stations will be set up in private, enclosed spaces at the Five Star Bank branches in Bath, Ovid; and Wayland and will be able to measure indicators for risk for high blood pressure, obesity, Type 2 diabetes, heart attack and stroke. Users will be able to connect with UR Medicine providers virtually.
Greater Rochester Health Foundation is proud to support this innovative effort to improve healthcare access in rural communities.
Read the full news release here; launch the 13 WHAM News segment here.


EE Pathways
EE Pathways Founder Wins Social Impact Award
Huge congratulations to EE Pathways Founder and CEO Karen James-Rogers, winner of the Social Impact Award at the University of Rochester’s Presidential Stronger as One Diversity Awards last month!
EE Pathways, located at 175 Genesee St. in Rochester, is on a mission to “inspire and energize historically disadvantaged communities to access resources during their physical and mental journey towards happier, healthier lives.” Click here to learn more about their work.
Lifespan of Greater Rochester
Health Affairs recently featured a case study of Lifespan of Greater Rochester Inc.’s Community Care Connections program and how it’s implementing a new Medicare policy designed to create more integrated care teams that provide patients with comprehensive, whole-person care leading to improved health equity, better health outcomes, and much-needed support for caregivers.
“Since 2016, Lifespan of Greater Rochester has been testing an integrated, whole-person care model through the implementation of the Community Care Connections (CCC) program, which provides services for older adults with complex social and medical needs. CCC employs social work case managers and licensed practical nurse health care coordinators to provide clients and caregivers with individually tailored and holistic services to address a range of social needs, as well as support coordinating and navigating their medical care.”
Health Affairs is a peer-reviewed journal exploring health policy issues of current concern in domestic and international spheres. Launch the full article here.

Faith Leaders Roundtable & YWCA
Health Foundation staff were invited to attend a Community Reception celebrating the completion of several living spaces for women who reside in the long-term housing at YWCA of Rochester & Monroe County.
Led by the The Faith Leaders Roundtable, volunteers, residents, staff and YWCA board members worked together to transform the shared spaces and kitchens on three floors at the YWCA to make the common areas more welcoming and comfortable.
Abundant Life Faith Center
Abundant Life Faith Center, now in the second year of their “Walking the Walk” initiative (also supported by Common Ground Health), produced a new video to share their stories of success and provide updates to the community on their efforts.
Guided by community voice, the goal of Walking the Walk is to expand reach, education, and support to a larger population of marginalized and underrepresented groups in our community around physical and mental health. Activities include an expanded blood pressure initiative, walking, yoga, meditation groups/classes, and more.
Abundant Life is also part of the Interdenominational Health Ministry Coalition. Click here or on the image to launch the video.

Indigenous Health Coalition Launches During Indigenous Peoples’ Month With Support from Common Ground Health
After more than an year of planning, a listening tour, and gathering information and interviews, the Indigenous Health Coalition held their inaugural meeting in November of 2023. Led by a small group of local Indigenous advocates, the coalition is open to and inclusive of any Indigenous people in the region and aims to ensure Indigenous health equity in its work, with support from Common Ground Health, the region’s health planning organization.
Common Ground Health also convenes regular meetings with the African American Health Coalition as well as the Latino Health Coalition. If you have questions or would like to stay up to date on what the coalition is up to, please reach out to Hannah Shippee at Common Ground Health, or click here for general information.
Mercy Flight


BreatheDeep
For Mental Health Awareness Month, May, 2023, we’re shining a spotlight on grantee partner BreatheDeep.
BreatheDeep recently invited Health Foundation Senior Program Officer Monica Brown to join a podcast created by Peer Ambassadors to highlight key mental health issues for youth, people of color, and the community at large. Monica spoke with Peer Ambassadors Josiah, Jaylyn, and Righteous. Dr. Silas, founder of BreatheDeep also joined the conversation.
Peer Ambassadors regularly produce “Just Breathe” podcasts with community members with an emphasis on youth impact and resources. Click here to launch the podcast.
BreatheDeep provides restorative wellness information and resources to help marginalized communities. Visit their website to learn more.

WellVentions Job Ready & Career Exposure Program
EE Pathways
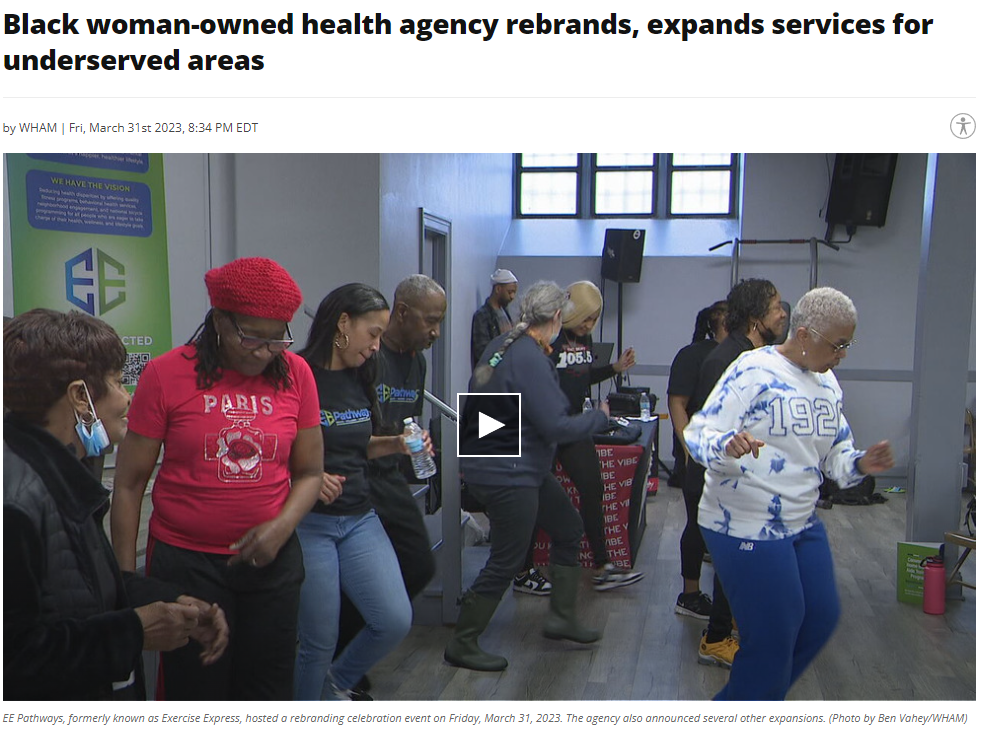
Congratulations to EE Pathways, formerly Exercise Express, on a successful rebranding event on March 31, 2023.
EE Pathways, located at 175 Genesee St., in Rochester, is on a mission to “inspire and energize historically disadvantaged communities to access resources during their physical and mental journey towards happier, healthier lives.”
The rebranding and expansion of services was recently featured on 13 WHAM News: Black woman-owned health agency rebrands, expands services for underserved areas: “We are about more than just exercise, it’s about finding multiple paths to wellness,” said Latisha McCray, the director of operations and programming at EE Pathways. “It’s needed in our community. A lot of the people in our community don’t always realize it’s very simple to take your health into your own hands.”
Flower City Noire Collective
Communications Officer Tiana Flynn and Program Officer Chiara Smith speak with founders Tonya Noel and Kristen Walker about how they fulfil the mission of Flower City Noire Collective “to elevate women of color in their communities using a holistic approach” through youth mentorship, supportive housing, community gardens and more.
Click here or on the image to launch the video.
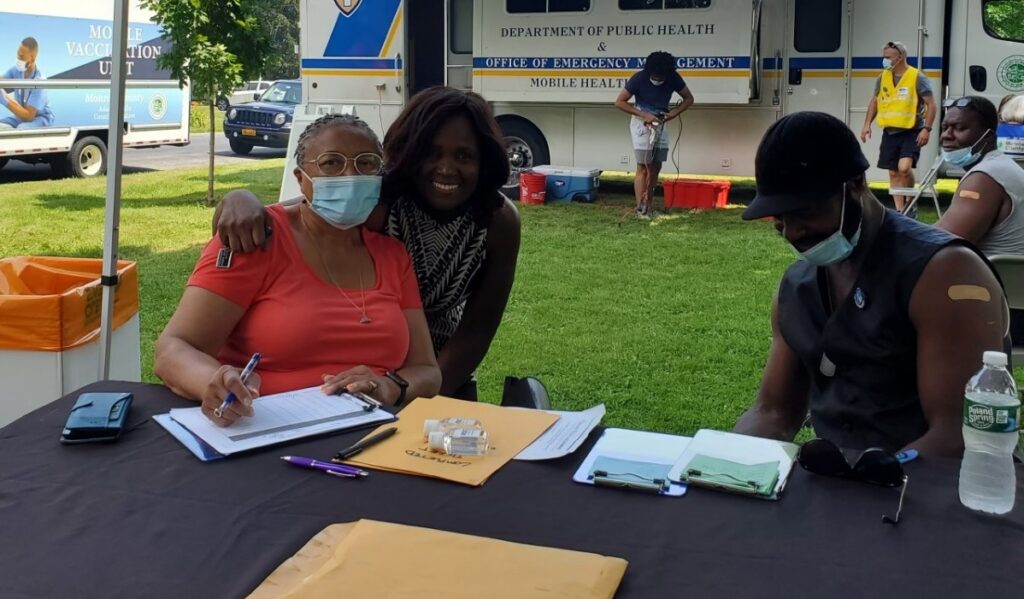
Partner Spotlight: Equitable Vaccine Distribution - Finger Lakes Vaccination Program
When the much-anticipated COVID vaccine arrived in the United States in early 2021, along with a renewed sense of optimism, the Governor promptly tasked the Finger Lakes Region with vaccinating 1.2 million people. In response, the Finger Lakes COVID-19 Vaccine Hub was formed to implement a comprehensive vaccination plan for the region.
The Finger Lakes COVID-19 Vaccine Hub collaborated with health departments, health care providers, community partners in Genesee, Livingston, Monroe, Orleans, Ontario, Seneca, Wayne, Wyoming and Yates Counties, with Common Ground Health, the region’s health research and planning organization, and with an advisory task force of 80 regional leaders. Hub partners collaborated to develop the Finger Lakes Vaccination Program, with a mission of ensuring the equitable, transparent, and efficient immunization of at least 70% of the adult residents of the Finger Lakes Region. Organized by the United Way of Greater Rochester and the Finger Lakes, in a matter of weeks the program secured nearly $1M in philanthropic funds from partners at Paychex, ESL Charitable Foundation, the Konar Foundation, Ralph C. Wilson, Jr. Foundation and Greater Rochester Health Foundation.
This unprecedented collaboration of public and private organizations has enabled large gains in vaccination rates in our region. When the work began, 31.5% of the population had received at least one dose of the vaccination, while today, more than 70% of the population has received a complete vaccine series. Through efforts coordinated by the Finger Lakes Vaccination Program and supported by philanthropic funds, 362 clinics were operated between April and September 2021, resulting in vaccination of over 33,000 individuals. With a central charge of equity in vaccine distribution, the program contributed to large increases in vaccination rates within the zip codes and populations most impacted by COVID and with least access to the vaccine.
To achieve these outcomes there were many obstacles that needed to be surmounted including the barrage of misinformation about COVID vaccines, mistrust resulting from histories of racism in medical institutions, as well as transportation, language and other access barriers disproportionately impacting lower-income urban as well as rural areas in our region. The Finger Lakes Vaccination Program developed and executed numerous strategies to address these barriers, including engaging in outreach and trust building in underserved communities, providing locally and culturally-tailored information and communications, and supporting vaccine administration within accessible, trusted community settings.
Project CERV
In this Grantee Spotlight video interview, learn more about Rochester Institute of Technology Project CERV via a Grantee Spotlight interview with Dr. Irshad Altheimer, Program Officer Chiara Smith, and Communications Officer Tiana Flynn.
Project CERV — which stands for Community Engagement to Reduce Victimization, is a collaborative, community-based violence intervention program targeting dispute-related violence. The program, part of the Center for Public Safety Initiatives at Rochester Institute of Technology (RIT), strives to help safety net providers reach and intervene with gun victims before new victimization events unfold.
Click here or on the image to launch the video.
HCR Cares
Congratulations to HCR Cares (a sister organization of HCR Home Care) for being featured in the Rochester Business Journal:
“HCR Cares will partner with more than 125 Rochester-area predominantly African American churches to help older adults in their congregations overcome barriers to using home health care services to improve their health outcomes.”
Learning Collaborative (Multiple Partners)
Fundamental to our Healthy and Equitable Futures work is the value of sharing, ceding, and leveraging power. Recognizing the importance of shifting power to families, the Health Foundation partnered with the National Parent Leadership Training Institute to build upon and leverage previous work to create a stakeholder learning collaborative and serve as a backbone for parent leadership and facilitation. A monthly Learning Collaborative launched virtually in 2021 during the COVID pandemic, is supported by more than 100 strategy partners, half of which are parents, including parents on 12 child-serving organization teams. With the support of 15 Parent Leader Facilitators and Soulstainable Living as DEI (diversity, equity, inclusion) consultant, stakeholders work to build and advance capacity in family leadership; racial diversity, equity, and inclusion; and social-emotional supports and connection so that Black and Latinx children ages zero to 8 in Monroe County are safe, supported, and thriving.

The Learning Collaborative serves as a mechanism to support organization and systems change efforts, and to address power inequities and advance racial justice. Organizations are working to leverage their strengths and their learnings to make policy and practice changes. The early learnings from this work have elevated the importance of parent voice in systems change, developing relationships within organizational teams so parents can meaningfully contribute, and creating space in the Learning Collaborative to discuss equity in systems change.
The Health Foundation remains on an intentional and humble journey with Parent Leaders and stakeholders to build relationships and infuse parent voice and decision making across the Healthy and Equitable Futures work, in support of trust-building and accountability.
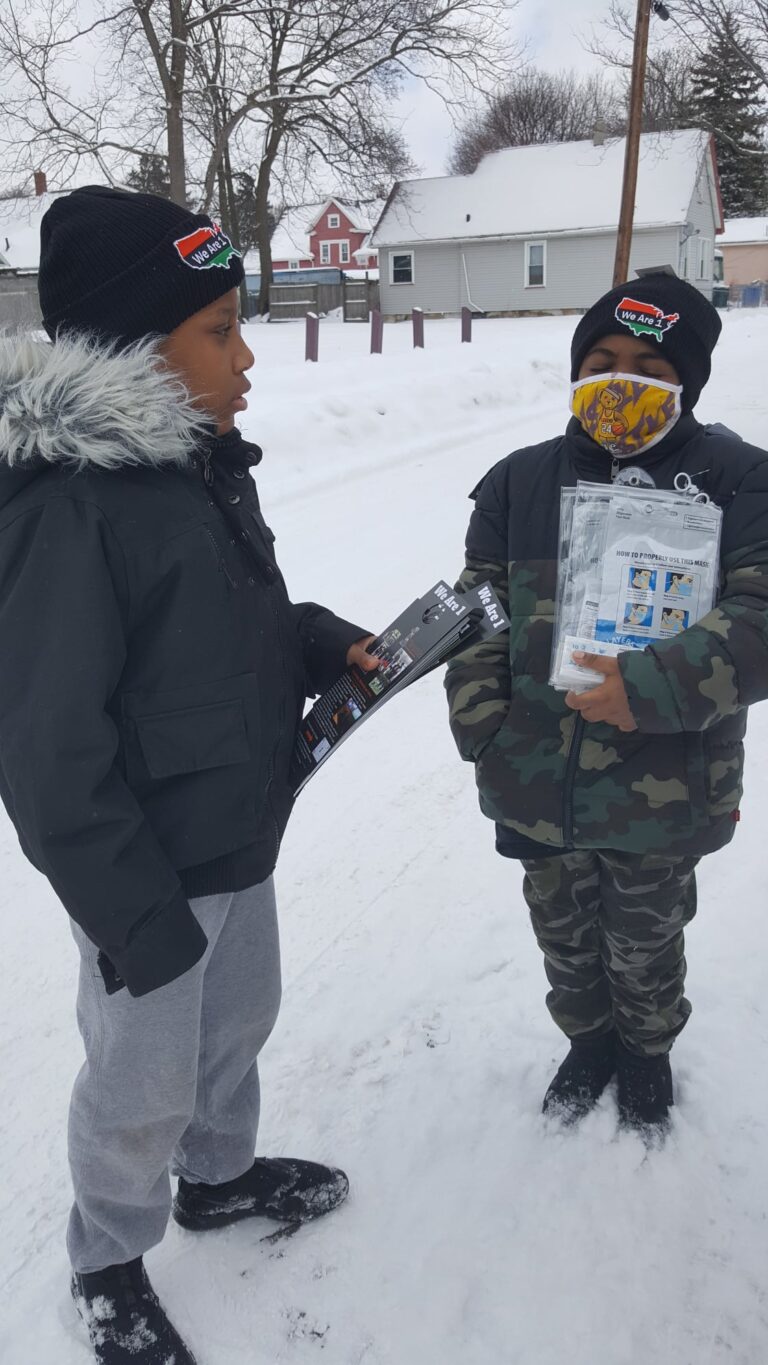
Player 1 Academy/We Are 1
Out of a desire to teach kids real-world life skills and provide tools to propel them to success, a new, Rochester-based non-profit is using video games, mentoring, education, and sports to help ensure that each child in their program will become a productive citizen who will make an enduring impact on their community.
We Are 1 is a strategic, “action-only movement” specifically designed to empower Black men, women, and children. Having adopted a universal code of unity, the organization’s efforts are “void of manipulation, jealousy, envy, anger, disgust, harm, and fear of one another.” We Are 1 engages in a structured, comprehensive series of approaches that allow Black people — as a whole — to gain control of their community by simultaneously supporting all areas of community members’ lives and well-being, as opposed to providing siloed services.
We Are 1’s face-to-face community engagement method brings an individual’s or a family’s resource needs directly to their doorstep. This approach has proven to be an effective tool for building genuine relationships with the community and fostering trust. Participating youth are trained to connect with residents in their neighborhood and collect information to help identify needs. In turn, this information informs the coordination and linkage to critical services including housing, food assistance, home maintenance, health care and other basic needs.
We Are 1 leverages a range of partnerships in the community, including: Rochester Housing Charities; Macy’s Department Store; Skate Luvers Roller Palace; Toastmasters International; and a behavioral health specialist from Monroe County.
The Health Foundation’s investment in the work of We Are 1 has proven to be imperative and impactful in 2021 as they reached nearly 2,000 community members — serving hot meals and distributing food to hundreds more through their Grill and Chill Community Cookouts and Lunch Da Block activities. In addition, more than 120 youth took part in boot camp and mentoring programs and benefitted from in-school supports and services in several local schools.
Latino Migrant Ministry (Wayne & Livingston Counties)
Despite the many challenges that migrant workers in Wayne and Livingston Counties encounter, this community finds remarkable resilience in their rich cultural heritage and social and religious ties.
Grappling with numerous threats to health and well-being, such as discrimination, language barriers, poverty, labor exploitation, housing and food insecurities, and anxieties over family separation or other stressors related to immigration status.

Additionally, many migrant workers are at an elevated risk for adverse COVID outcomes due to status as essential workers, higher density living conditions, barriers to accessing public health information, testing and healthcare, as well as social services or COVID relief resources. These adversities contribute to disproportionate experiences of trauma, mental health concerns, and public health needs.
The Latino Migrant Ministry operating through Our Lady of Guadalupe Church and in partnership with Nazareth College, seeks to support, sustain, and grow the quality of the essential services and supports provided for the members of these marginalized, often isolated communities of farm workers and their families.
The Latino Migrant Ministry provides a safe, trusted space and respite opportunities for farm workers and their families to engage in restorative cultural empowerment, educational opportunities, and well-being activities and retreats. Specific programs foster youth activities, community engagement, support for women, and English language classes, among others. With the Health Foundation’s support, the Latino Migrant Ministry has been able to engage more members of this community and enhance the quantity and quality of healthy foods offered during activities. In 2021, the Ministry served more than 100 families, adults, children, and youth.

Just Cause
People born outside the U.S. make up a vital part of the fabric of our communities, heavily contributing to the number of essential workers and those whose jobs support critical food and supply chains throughout the entire Finger Lakes Region.
The latest U.S. Census data estimates the foreign-born population in Monroe County at around 67,000. That’s nearly one in 10 county residents, with around two-thirds being U.S. citizens and two-thirds having been in the country for more than 10 years.
Whether documented or not — this community is more likely to suffer adverse health outcomes linked with inequities. New Americans often contend with the burden of xenophobia as well as racial and economic bias. These multiple layers of oppression can increase their social, emotional, and physical health vulnerabilities — making immigration status itself a social determinant of health. While much work is needed to dismantle the systems and social constructs that fuel this discrimination, the Immigrants’ Rights Program, created by Just Cause (formerly Volunteer Legal Services of Monroe, Inc.), seeks to interrupt the cycles that perpetuate these inequities while ensuring the safety, health, and civil rights of children and families who have immigrated to the U.S.
Access to legal supports, linkages to supportive services, and preventive medical care can reduce the impact of isolation, challenge illegal workforce practices, and facilitate integration with the larger community. The program addresses multiple social determinants of health around housing, domestic violence protections, and health care services for a population that can be greatly marginalized by language barriers, transportation barriers, and fear regarding status.
The Greater Rochester Health Foundation’s investment in this program supports key components such as: staffing, supplies, and court fees to ensure that attorneys, staff, and volunteers have what they need to provide these important services. Through the Immigrants’ Rights Program, more than 1,000 individuals,
families, and children benefited from legal education, direct legal representation, or legal counseling in 2021. The Health Foundation is proud to support these critical efforts.
BluePrint Geneva
Healthy communities that thrive are built on many factors, one of which is access to healthy food. Geneva, New York has been identified by the U.S. Department of Agriculture as a designated Food Scarcity Zone. Like too many of our communities, the limited number of grocery stores and the subsequent closing of small chain markets during the pandemic left many community members without access to a full range of healthy food options.
Yet, when communities collaborate, abundance can be created. BluePrint Geneva, Inc. began its journey as a nonprofit in 2016 with the goal of capitalizing on the bountiful agricultural enterprise in the area to increase food access and affordability for under-resourced neighborhoods and community members within the City of Geneva.
In 2020, they began to partner with local farmers such as Schrader’s, a woman-owned butchery, to establish a meat co-operative that would improve the community’s access to high-quality, affordable meat and other products. Through this innovative co-op, BluePrint Geneva successfully launched the Healthy Food Direct project in March of 2021. Within nine months, the project had served more than 130 unique households and completed hundreds of deliveries. The collaborating partners continue to grow, as do the types of fresh and reduced-price foods they provide to the community.

The Greater Rochester Health Foundation’s grant was awarded to support core project components and startup needs. It is often the basics, such as EBT access technology and cold storage unit purchases that impede grassroots organizations from furthering their critical work. Supported by the Health Foundation’s
investment and fueled by deep knowledge of the community, BluePrint staff and volunteers, farmers, and other partners are working to expand the food options and reach of the co-op to increase healthy and affordable food access in Geneva.